Shoulder Complex and Common Impairments
Shoulder pain is reported to occur in up to 21% of the general population, with 40% persisting for at least 1 year at an estimated annual cost of $39 billion. Shoulder impingement is the most prevalent diagnosis accounting for 40 to 65% of reported shoulder pain, whereas traumatic shoulder dislocations account for an additional 15 to 25% of shoulder pain. The persistent nature of shoulder pain may be the result of degenerative changes to the shoulder’s capsuloligamentous structures, articular cartilage, and tendons as the result of altered shoulder mechanics. As many as 70% of individuals with shoulder dislocations experience recurrent instability within 2 years and are at risk of developing glenohumeral osteoarthritis secondary to the increased motion at the glenohumeral joint. Degenerative changes may also affect the rotator cuff by weakening the tendons with time through intrinsic and extrinsic risk factors, such as repetitive overhead use (>60 degrees of shoulder elevation), increased loads raised above shoulder height, and forward head and rounded shoulder posture, as well as altered scapular kinematics and muscle activity (altered force-couple relationships). These factors are theorized to overload the shoulder muscles, especially the rotator cuff, which can lead to shoulder pain and dysfunction. Given the cost, rate of occurrence, and difficult resolution of shoulder pain, exercise solutions that address these factors are essential in preventing shoulder injuries.
The unique anatomy of the shoulder girdle enables the joint to balance maximum mobility while maintaining stability through dynamic and static stabilizing structures. Stability is derived primarily from the muscles about the shoulder girdle, and mobility is permitted by the relatively loose capsuloligamentous structures. Stability is maintained by the static and dynamic stabilizers that must work together to create the synchronous motion that allows for the high velocities, large torques, and precise timing such as full circumduction during swimming and powerful throwing motions that generate forces at the shoulder in excess of three times one’s body weight. There are many bones, muscles, and ligaments making up the shoulder girdle.
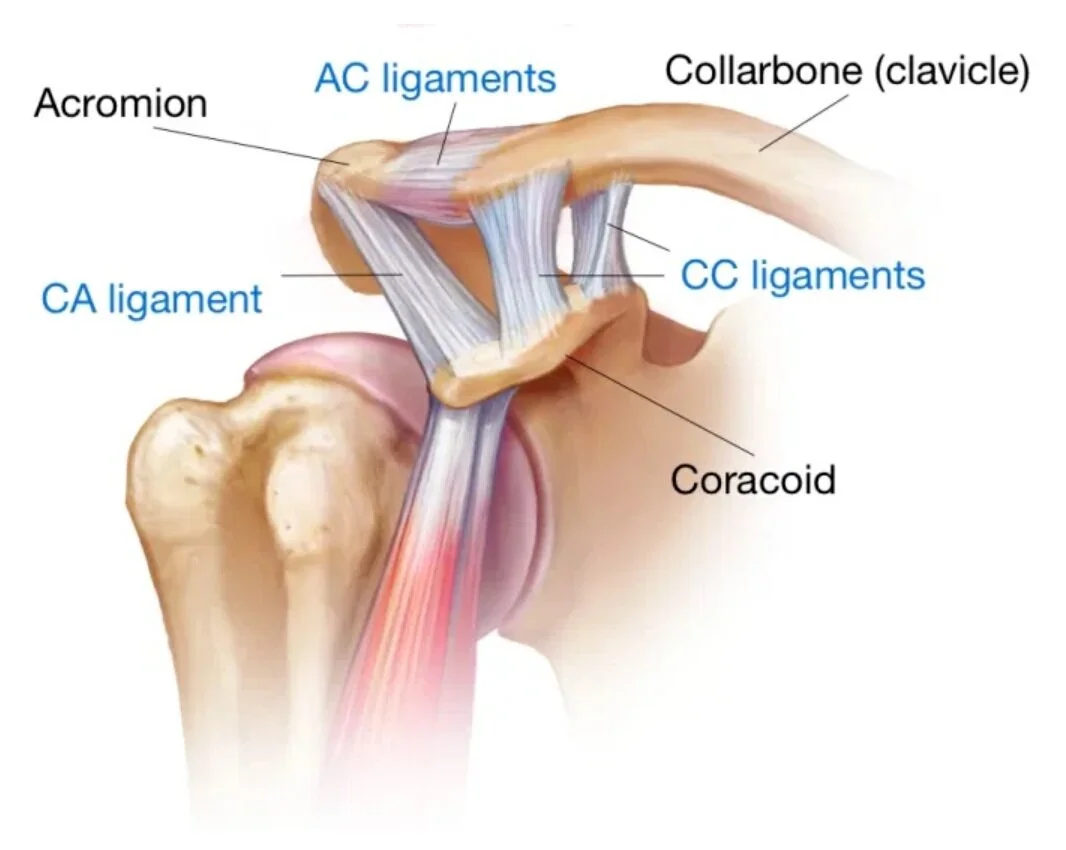
The shoulder girdle has the greatest range of motion of any joint in the body and refers specifically to the articulations between the humerus, scapula, clavicle, rib cage (thorax), and sternum that make up the glenohumeral (GH), acromioclavicular (AC), sternoclavicular (SC), and scapulothoracic joints. Below the shoulder are the lumbo-pelvic-hip complex (LPHC), which includes the lumbosacral, sacroiliac, and iliofemoral joints. These structures anchor many of the major myofascial tissues, especially the latissimus dorsi, which functions as a powerful shoulder adductor and internal rotator. Thus, dysfunction at the LPHC can affect proper shoulder function and vice versa.
The glenohumeral joint is a ball-and-socket articulation between the head of the humerus and the glenoid of the scapula, that affords a vast range of motion and great mobility that sacrifices stability. The glenoid surface is one third to one fourth the size of the humeral head, producing low contact area and low stability. The joint must rely on the static and dynamic stabilizers for its stability as well as for its motion. The static stabilizers include such structures as the glenoid labrum and the glenohumeral joint capsule consisting of two major ligaments, the middle and inferior glenohumeral ligaments. Toward the end ranges of glenohumeral motion, these ligaments tighten to limit motion and provide functional stability. However, in midranges of shoulder motion, these ligaments are relatively lax, and the joint must rely heavily on the musculature that surrounds the joint for dynamic stability.
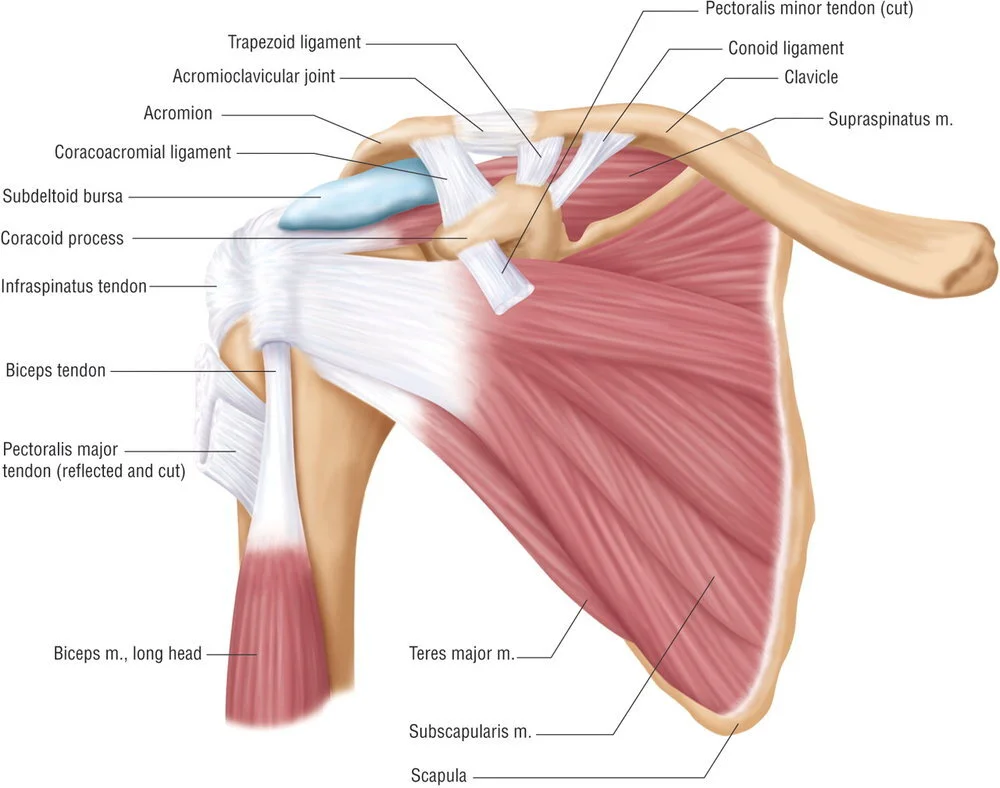
The dynamic stability of the glenohumeral joint is dependent on the musculature that surrounds the joint, including the rotator cuff and the scapular stabilizers. The rotator cuff is the primary steering mechanism of the glenohumeral joint. The rotator cuff is made up of the supraspinatus and subscapularis anteriorly, with the infraspinatus and teres minor posteriorly. The supraspinatus initiates the first 15 degrees of shoulder abduction followed by deltoid activation for the remainder of the arc of motion. The deltoid and supraspinatus work together in a force-couple to control the humeral head in the frontal plane. The main action of the subscapularis is medial rotation of the humerus while also being the primary stabilizer and humeral head depressor. The infraspinatus and teres minor externally rotate the glenohumeral joint and decelerate the humerus during internal rotation. The subscapularis and posterior rotator cuff function together in a force-couple controlling the humeral head in the transverse plane.
Function of the Scapula
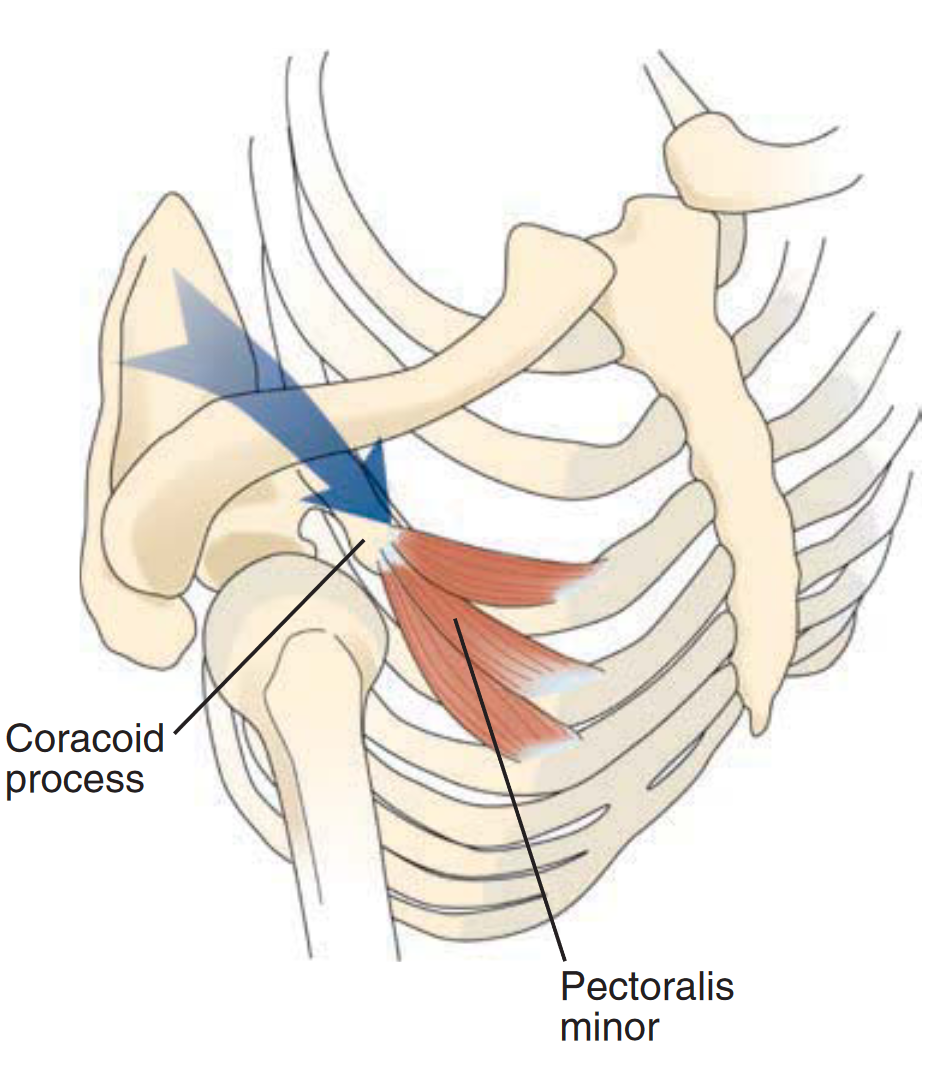
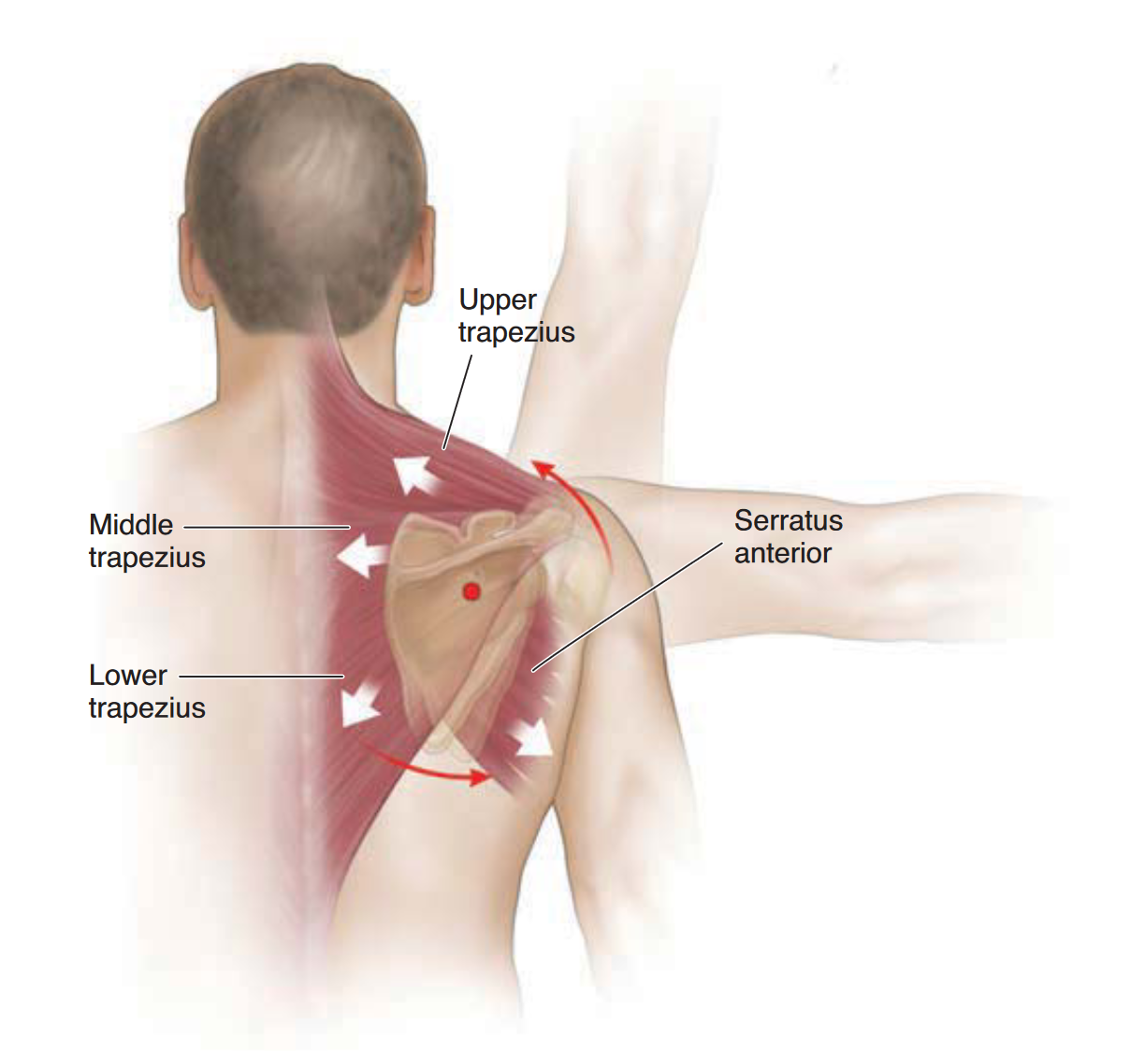
The scapulothoracic articulation allows shoulder movement beyond the 120 degrees of elevation provided by the glenohumeral joint. It also plays an important role in providing motion and shoulder girdle stability through the 17 muscles that attach to the scapula. When these muscles function properly, they provide a stable base for the humerus to glide on and allow for an efficient transfer of force from the lower extremities and trunk. This is accomplished through force couples of the upper, middle, and lower trapezius as well as the serratus anterior. The effectiveness of these force couples is reliant on the presence of optimal length-tension relationships between opposing muscles. Decreases in force production may lead to disruption in normal muscle synergies and decrease the ability of a force-couple to functionally control joint motion. For example, tightness in the pectoralis minor, which inserts on the coracoid process of the scapula, will limit the effectiveness of the serratus anterior. Therefore, the pectoralis minor plays an important role in scapula malposition as it can pull the scapula into a more protracted and anteriorly tilted position.
Common Shoulder Injuries and Associated Movement Deficiencies
Shoulder injuries can be broadly categorized into those that affect the rotator cuff muscles or those that affect the capsuloligamentous structures of the shoulder. Rotator cuff conditions such as strains, ruptures, and tendinopathies account for approximately 75 to 80% of shoulder injuries. Rotator cuff strains occur when a muscle group is overexerted, causing microdamage within the muscle belly and tendon, resulting in immediate inflammation and decreased muscle function. In contrast, injuries to the capsuloligamentous structures lead to deficits in the passive stabilizing structures of the shoulder such as the anterior, posterior, or inferior glenohumeral ligaments and the glenoid labrum. These injuries are devastating to the ability of the shoulder to facilitate function of the upper extremity in reaching forward or performing overhead tasks.
Shoulder Impingement
Subacromial impingement syndrome (SAIS) is a common diagnosis broadly defined as compression of the structures that run beneath the coracoacromial arch, most oft en from a decrease in the subacromial space. The impinged structures include the supraspinatus and infraspinatus tendons, the subacromial bursa, and the long head of the biceps tendon. Repetitive compression of these structures with the overhead motions required of many sports and activities of daily living can lead to irritation and inflammation. In turn, prolonged inflammation can cause muscular inefficiency, specifically affecting the rotator cuff muscles. SAIS may be the result of bony deformity of the acromion, underlying rotator cuff weakness, shoulder instability, or scapular dyskinesis. Rotator cuff weakness and shoulder instability results in excessive superior and anterior translation and inadequate external rotation of the humeral head, limiting clearance of the greater tuberosity under the acromion process. Decreases in the normal scapular upward rotation and external rotation of the humerus combined with posterior tilting on the thorax cause a decrease in the physiologic space under the coracoacromial arch. Many of these faulty joint motions may be caused by a muscular imbalance or a disruption in force couple relationships. If these faulty motions are consistently repeated, the resulting decrease in space can lead to impingement of the structures running through the coracoacromial arch. Decreased upward rotation and posterior tilting of the scapula have been shown to occur as the result of forward head posture, forward shoulder posture, or thoracic kyphosis. With time, this altered initial position is thought to place the serratus anterior, lower trapezius, subscapularis, and posterior rotator cuff at a mechanical disadvantage that can cause weakness and is referred to as the upper crossed syndrome. This altered position of the scapula is thought to result in a decreased subacromial space that could potentially damage the aforementioned structures. This impingement or the resulting stresses can damage the rotator cuff, reducing the function of the cuff muscles to suboptimal levels. The resulting alteration in glenohumeral mechanics places the shoulder at an increased risk of injury, especially when combined with overhead activity.
Shoulder Instability
Shoulder instability results from many different mechanisms, but regardless of the mechanism, instability most often manifests itself as anterior or multidirectional. These forms of instability differ greatly in terms of the involved structures and injury mechanisms. Even though the exact injury mechanism may differ, all forms of shoulder instability may occur by means of a traumatic injury mechanisms associated with improper mechanics and poor conditioning. The most common is traumatic anterior instability as the result of an abducted and externally rotated arm that might occur during a fall on an outstretched arm or reaching behind and to the side to tackle someone. This results in damage to the anterior/inferior glenohumeral ligament and often the glenoid labrum. The resulting instability usually leads to significant disability with overhead activities that in most cases requires surgical repair. Shoulder instability may also have an insidious onset as the result of repetitive overhead motion or congenital hypermobility. Repetitive overhead motion of an abducted arm into extreme external or internal rotation results in deformation and failure of the static stabilizers. This tissue deformation of the static structures is often termed micro, multidirectional, or atraumatic instability. If overhead motion continues and the previously discussed dynamic stabilizers are not functioning, then rotator cuff fatigue or chronic injury may result. It is generally accepted that tissue deformation occurring from injury causes decreased proprioceptive ability secondary to partial deafferentation of the joint and its stabilizing structures. Alteration of the shoulder’s neuromuscular control can lead to an asynchronous firing pattern, leading to a maltracking glenohumeral joint, which in and of itself defines shoulder dysfunction. This dysfunction leads to increased distraction forces and tensile stress on the rotator cuff. This process leads to further instability as the static stabilizers are stretched out, the dynamic structures become increasingly weak, and the mechanoreceptors respond slower, thus compromising shoulder performance in the attempt to avoid injury.
Closed-Packed Position and Behind the Neck Exercises
The closed-packed position is when the joint surfaces are maximally fit and the capsule and ligaments have the least ability to lengthen. In this position the joint surfaces are compressed and the joint possesses its greatest stability, but least amount of mobility. So to picture this in relative terms, hold a towel at both ends and twist it in opposite directions and notice how as the towel twists your hands move closer together. The joint is compressed by virtue of the fact that the capsule and ligaments are spiralized and tense. In this situation the surface cannot be separated by distractive force, but the position does subject the joint to possible damage because of the compressive and shear stresses. To be clear, it is not the position that is dangerous, but the direction and amount of external force applied to the joint/limb that will determine the level of risk. To decrease stress on the joint and decrease the risk of injury the joint should be placed in the loose-packed position. This is the position where the joint is least fit and has the most extensibility in the capsule and ligaments. For example, many people try to strengthen their latissimus dorsi and deltoids by performing behind the neck pulldowns or presses. This forces one to place their shoulder into the closed-packed position (shoulder external rotation, abduction, and maximal elevation). However, a simple modification is to pull or press the load in front of the shoulder (front lat pulldowns or front shoulder presses), which avoids the closed-packed position and provides a safer alternative to avoid injuries in the future.
Distal Injuries associated with shoulder impairment
As mentioned earlier, because of the connectivity of the structures and tissues of the kinetic chain, shoulder dysfunction can migrate toward or stem from imbalance or injury in the LPHC, knee, and foot and ankle complex, which includes low back pain; sacroiliac joint dysfunction; hamstring complex, quadriceps, and groin strains; patellar tendonitis; iliotibial band (IT-band) tendonitis; plantar fasciitis; Achilles’ tendonitis; and posterior tibialis tendonitis (shin splints).
Shoulder injuries can significantly limit participation in recreational and competitive athletics. Common shoulder injuries such as impingement syndrome and instability are routinely correlated with movement dysfunction. As with the other regions of the body, identification of movement dysfunction using clinical screens provides an efficient way to address muscle imbalances. Focused corrective exercise programs progressing from inhibition–lengthening–activation–integration are likely to address these muscle imbalances of the shoulders.
REFERENCES
1. Bongers PM. The cost of shoulder pain at work. BMJ. 2001
2. Urwin M, Symmons D, Allison T, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Di. 1998
3. Van Der Heijden G. Shoulder disorders: a state of the art review. Baillieres Best Pract Res Clin Rheumatol. 1999
4. Johnson M, Crosley K, O’Neil M, Al Zakwani I. Estimates of direct health care expenditures among individuals with shoulder dysfunction in the United States. J Orthop Sports Phys Ther. 2005
5. Van Der Windt DA, Koes BW, Boeke AJ, Deville W, De Jong BA, Bouter LM. Shoulder disorders in general practice: prognostic indicators of outcome. Br J Gen Pract. 1996
6. Hovelius L. Shoulder dislocation in Swedish ice hockey players. Am J Sports Med. 1978
7. Hovelius L. Incidence of shoulder dislocation in Sweden. Clin Orthop Relat Res. 1982